By Aaron Webb, Acadian Physician Assistant
According to the Asthma and Allergy Foundation of America, approximately 25 million Americans have asthma. This equates to about 1 in 13 Americans, including 8 percent of adults. It affects 7 percent of children and is the leading chronic disease in children.
The CDC reports that while the rate of emergency department (ED) visits with a primary diagnosis of asthma remained stable from 2010 through 2018, the visit rate (per 10,000 population) was significantly higher among children at 88.1, than among adults at 42.1. The rate among women was 50.4, higher than among men at 31.1.
There is no cure for asthma, so being aware of triggers, preventing and managing mild symptoms, and controlling exacerbations with medication is extremely important.

Preventing Potential Asthma Attacks
- Identify asthma triggers
Certain triggers can set off asthma symptoms. These include:
-
- Air pollution
- Smoking
- Cold, flu, or other viruses
- Genetics
- Pets
- Household chemicals
- Dust
- Allergies
- Exercise
- Artificial fragrances
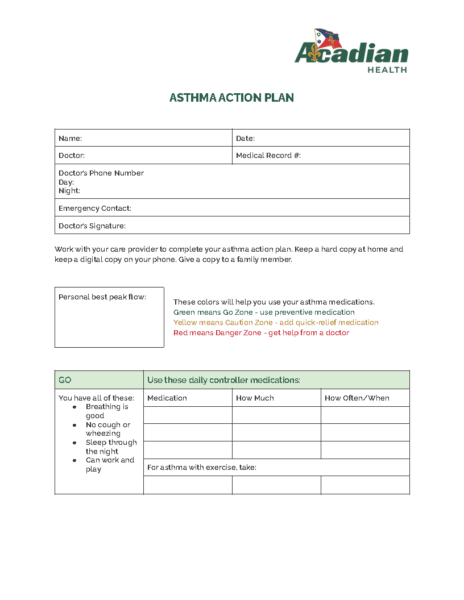
Keep track of your symptoms in an asthma diary (see a sample here) for several weeks. Record all the environmental and behavioral circumstances that occur throughout your day. When you have an asthma attack, check the diary to see what may have led to it. Some common asthma triggers, like molds and cockroaches, aren’t always obvious. Ask your asthma specialist about tests to find the allergens you respond to.
If you have exercise-induced asthma, are planning a heavy workout, or plan to exercise in cold, humid, or dry air, plan ahead to prevent an asthma attack. Follow your doctor’s advice on asthma treatment (usually by using an albuterol inhaler before you exercise).
- Allergy-proof your spaces and stay away from allergens
Whether you’re at home, work, or traveling, there are things you can do to allergy-proof your environment and lower your chances of an asthma attack. Allergen exposure can increase the inflammation in your airways, making an attack more likely. Limit exposure to all sources of smoke, including tobacco, incense, candles, fires, and fireworks. Don’t allow smoking in your home or car, and avoid public places that permit it. Bring your own bedding and pillows when traveling in case your lodging only supplies feather pillows and down comforters, which can house dust mites and cause asthma symptoms.
- Prevent colds
Do what you can to stay well. Avoid close contact with people who have a cold or the flu, because these viral infections can make your asthma symptoms worse. Wash your hands frequently if you have been exposed to someone with a viral infection.
Managing Asthma
- Consider immunotherapy allergy shots and get your vaccinations
If your doctor finds that you have allergies, allergy shots (immunotherapy) may help prevent allergy symptoms and keep your asthma from getting worse. With allergy shots, the doctor injects small doses of allergens under your skin on a regular schedule. Over time, your body may get used to the allergen and respond better when you’re exposed.
Get a flu shot every year to protect against the Influenza virus, which can worsen your asthma. Asthma makes you more likely to have complications from the flu, like pneumonia, and increases your chances of being hospitalized. Many people with asthma should get a pneumococcal vaccination to decrease your risk of getting pneumonia. Ask your healthcare provider if you should get it.
- Take your medications as prescribed
Long-term asthma medications are designed to prevent symptoms and attacks and should be taken every day, even if you don’t have symptoms. They’ll ease inflammation in your airways and keep your asthma under control, so it’s less likely to flare up. If side effects bother you, talk to your doctor about switching to another treatment.
-
Develop and follow your asthma action plan
Work with your healthcare provider to develop an action plan that includes key information on managing your asthma. Keep a rescue inhaler with you at all times. If you notice symptoms, check your plan for instructions on what medications to take. During an attack, the plan can tell you what medications will help and when it’s time to call the doctor.
- Use a home peak flow meter
A home peak flow meter shows how well air is moving through your lungs. During an attack, your airways narrow. The meter can let you know this is happening hours or days before you have any symptoms. This gives you time to take the medications listed in your treatment plan and possibly stop the attack before it starts. Contact your provider to obtain a prescription for a peak flow meter.
In 2016, asthma accounted for 9.8 million doctor’s office visits. With healthcare at home becoming a more common treatment option these days, the number of doctor’s office visits can be reduced, saving a patient time and increasing their comfort.
Our Acadian Health team members are well-equipped to help care for you when your asthma attacks. Call your healthcare provider and health plan to request access to Acadian Health to help you manage your next asthma attack in your home.
Sources:
- https://www.aafa.org/asthma-facts/
- https://www.webmd.com/asthma/guide/asthma-prevention
- https://www.stanfordchildrens.org/en/topic/default?id=management-and-treatment-of-asthma-90-P01694
- https://www.lung.org/lung-health-diseases/lung-disease-lookup/asthma/living-with-asthma/managing-asthma
- https://www.cdc.gov/asthma/asthma_stats/asthma-ed-visits_2010-2018.html